HSM2: Improvement of Patient Safety and Quality of Results through Computer-Assisted Surgery
The goal of the project is the investigation of new methods for computer-based, patient-specific 3D preoperative planning and surgical navigation of orthopedic interventions.
As part of the overall strategy of highly specialized medicine, the Government of Canton Zurich supports selected projects at the University of Zurich and its hospitals. Our project has been selected as one of seven projects for the second implementation phase (HSM II; 2015-2018) to promote outstanding achievements in knowledge, research and highly specialized medicine. In the project, the University hospitals (Balgrist, University Hospital, Children's Hospital) worked together with the University of Zurich and ETH Zurich.
The aim of this project is to establish a center for computer-assisted orthopedic surgery with a focus on direct clinical application on patients. The center's competencies will be in the generation of 3D anatomical models, 3D preoperative planning and computer simulation of bone and soft tissue pathologies, surgical navigation and 3D printing of anatomical structures. The center will be active in patient treatment, but also in teaching and further education. The project was successfully completed as described in the press-release.
Benefits for highly specialized medicine
For the patient, the project outcomes will result in greater precision in the indication and the execution of surgeries as well as lower anesthesia and operation times and consequently in lower complication and re-operation rates. In high-risk surgeries, such as spinal intervention, the risk of serious complications can be technically minimized through precision. Balgrist University Hospital has already demonstrated in studies that certain operations are only possible with the use of such technologies and that this method can sometimes deliver a better treatment outcome than conventional alternatives. This improves the quality of life and work capacity of patients with pathologies that are technically difficult to treat, which is of interest to the canton's entire population.
For the highly specialized surgery at the University Hospitals of Zurich, a new method especially for soft-tissue pathologies will be implemented to enable more precise preoperative planning, exact surgical execution and quantitative, technical success control. Computer-based planning will allow various surgical strategies to be evaluated, thus promoting the development of new surgical techniques. Surgeons will develop a more quantitative understanding of surgeries and a higher degree of certainty in planning and execution of surgeries. Surgeons will be trained in 3D thinking and acting, which will generally improve their surgical skills. The standardization and quantification of surgeries will contribute to quality assurance in the detection of planning and execution errors.
The project will enable Zurich to position itself as one of the world's leading clinical research lighthouses in the field of applied 3D planning and navigation of joint-preserving bone surgery.
Generation of 3D anatomical models of the patient
The generation (segmentation) of 3D anatomical models based on medical image data is an essential basis for higher-level computer-based approaches. Patient-specific models of soft tissue anatomy remain the greatest challenge, as their generation is time-consuming and tedious. In collaboration with the ETH Zurich, automatic segmentation methods for MRI images have been developed based on the concept of machine learning.
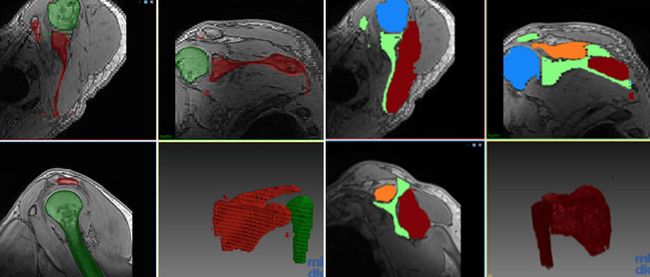
Figure 1: Segmentation of muscle and bone tissue in MR images
Initially traditional hand-crafted feature-based artificial intelligence techniques such as Random Forests were studied, leading to [16-1, 17-1]. Later, neural network approaches were developed as novel and more advanced techniques (Figure 1 D). Since the accuracy of these methods rely on the availability of annotated data, ETH Zurich investigated automatic-suggestion systems to intelligently suggest ideal images to annotate for highest accuracy gain [18-1]. The most prominent contribution in this direction was the introduction of a novel concept for step-by-step extension of advanced learning techniques to new anatomy [18-2]. In recent work we have shown that other muscles can be segmented based on very few approximate annotations. In future work, such segmentation methodology will form the basis of customizing generic musculoskeletal models to patient-specific images, in order to utilize in functional simulations and hence for surgical planning and decision making.
3D preoperative planning and surgical navigation
3D preoperative planning uses the 3D anatomical models of a patient to simulate surgical intervention on the computer step by step, until the desired surgical objective is realized. The results of the simulation will then provide the basis for surgical navigation. The goal of surgical navigation is to support the surgeon in the operation in such a way that he can execute the intervention with high precision and according to the preoperative planning. One concept of surgical navigation are patient-specific instruments (PSI), which are designed on the computer and tailored to the patient and his intervention. PSI are manufactured using 3D printing technology, sterilized and positioned directly on the corresponding anatomy in the surgery. The research within the HSM2 projects was built on existing technology, which was originally developed by us for the 3D planning and surgical navigation of bone malunions.
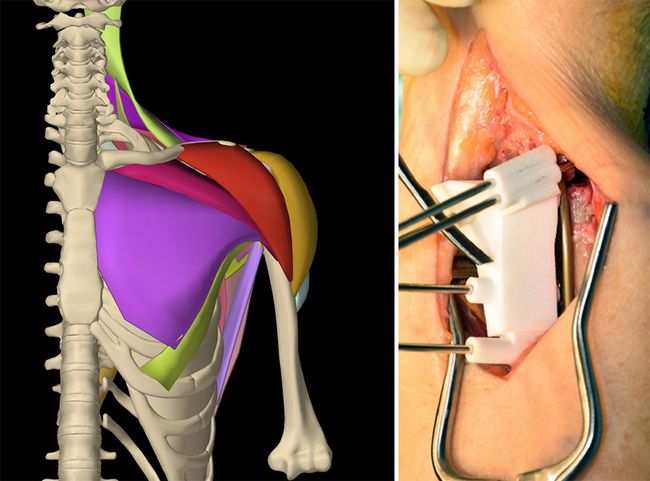
Figure 2: (A) HSM2 shoulder model. (B) patient-specific instruments for the surgical navigation of osteosyntheses.
A major part of the project [18-3,18-6] was dedicated to the development of a comprehensive dynamic model of the shoulder (Figure 2 A), with the rotator cuff and all other relevant shoulder muscles - a total of over 25 muscles. This functional model can emulate muscle activations and the generated forces that lead to the motion of the musculoskeletal system. Given prescribed motion patterns, the model can find required muscle activations using inverse dynamics control. With the resulting activations and motion, the shoulder can be better represented and understood. In recent work under revision [18-3] these functional simulations are being evaluated using public datasets of motion capture data as well as EMG recordings of individuals during shoulder motion. This requires the mapping of our generic/atlas functional model to individual, forming the first steps and a baseline for subject-specific modelling. Moreover, the use of 3D preoperative planning and patient-specific instrument navigation for bone tumor resection surgery was also brought into clinical practice [16-6]. A newly-developed MRI-CT fusion technique permitted the integration of soft tissue (tumor), with a case study showing superior precision of navigatated tumor resections compared to the conventional free-hand approach [16-6].
Within the course of the project, more than 400 patients were treated and 15 clinical studies were conducted to demonstrate feasibility and efficiency of the methods.
Publications
2015
[15-1] Vlachopoulos L, Dünner C, Gass T, Graf M, Goksel O, Gerber C, Szekely G, Fürnstahl P. Computer algorithms for 3D measurement of humeral anatomy - analysis of 140 paired humeri. Journal of Shoulder and Elbow Surgery, 2015. 25(2): 38-48. Impact Factor: 3.089 (5-years)
[15-2] Hingsammer A, Vlachopoulos L, Meyer D, Fürnstahl P. Three-Dimensional Corrective Osteotomies of Mal-united Clavicles - is the contralateral anatomy a reliable template for reconstruction? Clinical Anatomy, 2015. 28(7): p. 865-871. Impact factor: 1.615 (5 year)
2016
[16-1] J. Thoma, F. Ozdemir, O. Goksel: "Automatic Segmentation of Abdominal MRI Using Selective Sampling and Random Walker", In W Medical Computer Vision, Lecture Notes in Computer Science LNCS 10081: 83-93, 2016. Impact factor: not listed in Journal Citation Report
[16-2] F. Ozdemir, E. Ozkan, O. Goksel: "Graphical Modeling of Ultrasound Propagation in Tissue for Automatic Bone Segmentation", In MICCAI, Lecture Notes in Computer Science LNCS 9901: 256-264, 2016. Impact factor: not listed in Journal Citation Report
[16-3] Schweizer A, Mauler F, Vlachopoulos L, Nagy L, Fürnstahl P. Computer-Assisted 3-Dimensional Reconstructions of Scaphoid Fractures and Nonunions With and Without the Use of Patient-Specific Guides: Early Clinical Outcomes and Postoperative Assessments of Reconstruction Accuracy. Journal of Hand Surgery, Am, 2016. 41(1): p. 59-69. Impact factor: 1.890 (5-years)
[16-4] Tschannen M, Vlachopoulos L, Gerber C, Szekely G, Fürnstahl P, Regression Forest-Based Automatic Estimation of the Articular Margin Plane for Shoulder Prosthesis Planning. Medical Image Analysis, 2016. 31: p. 88-97. Impact factor: 5.012 (5-years)
[16-5] Vlachopoulos L, Schweizer A, Meyer DC, Gerber C, Fürnstahl P. Three-dimensional corrective osteotomies of complex malunited humeral fractures using patient-specific guides. J Shoulder Elbow Surg, 2016. 25(12): p. 2040-2047. Impact Factor: 3.089 (5-years)
[16-6] Jentzsch T, Vlachopoulos L, Fürnstahl P, Müller D, Fuchs B. Tumor resection at the pelvis using three-dimensional planning and patient-specific instruments: a case series. World Journal of Surgical Oncology, 2016. 14(1): p. 249. Impact factor: 1.716 (5-years)
[16-7] Schenk P, Vlachopoulos L, Hingsammer A, Fucentese S, Fürnstahl P. Is the contralateral tibia a reliable template for reconstruction – A three dimensional anatomy cadaveric study. Knee Surgery, Sports Traumatology, Arthroscopy, 2016. Impact factor: 3.284 (5-years)
2017
[17-1] F. Ozdemir, N. Karani, P. Fürnstahl, O. Goksel: Interactive Segmentation in MRI for Orthopedic Surgery Planning: Bone Tissue, Int J Comp. Assisted Radiol. Surgery 12(6):1031-9, 2017. Impact factor: 1.86 (2016) / 1.86 (5-years)
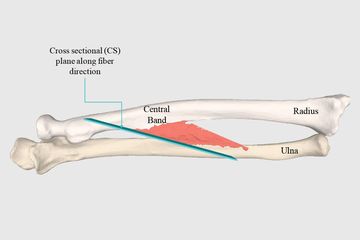
[17-2] F. Pean, F. Carrillo, P. Fürnstahl, O. Goksel: "Physical Simulation of the Interosseous Ligaments During Forearm Rotation", In Computer Assisted Orthopaedic Surgery, 2017. Impact factor: not listed in Journal Citation Report
[17-3] Wieser K, Fürnstahl P, Carrillo F, Fucentese S, Vlachopoulos L. Isometry of the Anterolateral Ligament: A Weight Bearing Computer Tomography Simulation. Arthroscopy: The Journal of Arthroscopic and Related Surgery. 2017 May;33(5): p. 1016-1023. Impact factor: 3.724 (2015) / 3.865 (5-years)
[17-4] Mauler F, Langguth C, Schweizer A, Vlachopoulos L, Gass T, Lüthi M, Fürnstahl P. Prediction of Normal Bone Anatomy for the Planning of Corrective Osteotomies of Malunited Forearm Bones Using a Three-Dimensional Statistical Shape Model. J Orthop Res. 2017 Dec; 35(12):2630-2636. Impact factor: 2.69 (2016) / 2.98 (5-years)
[17-5] Bauer D, Zimmermann S, Aichmair A, Hingsammer A, Schweizer A, Nagy L, Fürnstahl P. Conventional Versus Computer-Assisted Corrective Osteotomy of the Forearm: a Retrospective Analysis of 56 Consecutive Cases. J Hand Surg Am. 2017 Jun;42(6):447-455. Impact factor: 1.64 (2015) / 1.822 (5-years)
[17-6] Weigelt L, Fürnstahl P, Schweizer A. Computer-assisted corrective osteotomy of malunited pediatric radial neck fractures - Three-dimensional postoperative accuracy and clinical outcome. Journal of Orthopaedic Trauma, 2017. 31 (12): 436-441. Impact factor: 1.840 (2015) / 2.203 (5-years)
[17-7] Dietrich TJ, Agten CA, Fürnstahl P, Vlachopoulos L, Pfirrmann CWA. The Legend of the Luschka Tubercle and Its Association With Snapping Scapulae: Osseous Morphology of Snapping Scapulae on CT Images. AJR Am J Roentgenol. 2017 Jul;209(1): p. 159-166. Impact factor: 2.78 (2016) / 3.10 (5-years)
[17-8] Vlachopoulos L, Schweizer A, Meyer DC, Gerber C, Fürnstahl P. Computer-assisted planning and patient-specific guides for the treatment of midshaft clavicle malunions. J [17-9] Shoulder Elbow Surg. 2017 Aug; 26(8):1367-1373. Impact factor: 2.73 (2016) / 3.08 (5-years)
[17-10] Hirsiger S, Schweizer A, Miyake J, Nagy L, Fürnstahl P. Corrective Osteotomies of Phalangeal and Metacarpal Malunions Using Patient-Specific Guides: CT-Based Evaluation of the Reduction Accuracy. Hand (N Y). 2017. Impact factor: not listed in Journal Citation Report.
[17-11] Weigelt L, Fürnstahl P, Hirsiger S, Vlachopoulos L, Espinosa N, Wirth SH. Three-Dimensional Correction of Complex Ankle Deformities With Computer-Assisted Planning and Patient-Specific Surgical Guides. J Foot Ankle Surg. 2017 Dec; 56(6): 1158-1164. Impact factor: 1.35 (2016)
[17-12] Roner S, Vlachopoulos L, Nagy L, Schweizer A, Fürnstahl P. Accuracy and Early Clinical Outcome of 3-Dimensional Planned and Guided Single-Cut Osteotomies of Malunited Forearm Bones. J Hand Surg Am. 2017 Dec; 42(12):1031.e1-1031.e8. Impact factor: 1.64 (2015) / 1.822 (5-years)
[17-13] Carrillo F, Vlachopoulos L, Schweizer A, Nagy L, Snedeker J, Fürnstahl P. A Time Saver: Optimization Approach for the Fully Automatic 3D Planning of Forearm Osteotomies. In: Image Computing and Computer-Assisted Intervention (MICCAI) 2017. Lecture Notes in Computer Science, vol 10434. Springer. Impact factor: not listed in Journal Citation Report
[17-14] Vlachopoulos L, Carrillo F, Gerber C, Székely G, Fürnstahl P. A Novel Registration-Based Approach for 3D Assessment of Posttraumatic Distal Humeral Deformities. J Bone Joint Surg Am. 2017 Dec 6;99(23). Impact factor: 4.6 (2016) / 6.1 (5-years)
2018
[18-1] F. Ozdemir, Z. Peng, C. Tanner, P. Fürnstahl, O. Goksel: “Active Learning for Segmentation by Optimizing Content Information for Maximal Entropy”, In Deep Learning in Medical Image Analysis, Lecture Notes in Computer Science LNCS 11045: 183-191, 2018.
[18-2] F. Ozdemir, P. Fürnstahl, O. Goksel: “Learn the New, Keep the Old: Extending Pretrained Models with New Anatomy and Images”, In MICCAI, Lecture Notes in Computer Science LNCS 11073: 361-369, 2018.
[18-3] F. Pean, C. Tanner, C. Gerber, P. Furnstahl, O. Goksel: “A comprehensive and volumetric musculoskeletal model for the dynamic simulation of the shoulder function”, Computer Methods in Biomechanics & Biomedical Eng., in review (minor revision), 2019.
[18-4] M. Ciganovic, F. Ozdemir, F. Pean, P. Fuernstahl, C. Tanner, O. Goksel: "Registration of 3D Freehand Ultrasound to a Bone Model for Orthopaedic Procedures of the Forearm", Int J Comp Assisted Radiology & Surgery 13(6):827-836, 2018. IF: 1.96
[18-5] M. Ciganovic, F. Ozdemir, M. Farshad, O. Goksel: "Deep learning techniques for bone surface delineation in ultrasound", In SPIE Medical Imaging 10955-33, 2019, accepted.
[18-6] F. Péan, P. Fürnstahl, O. Goksel: “A musculoskeletal model of the shoulder combining multibody dynamics and FEM using B-Spline elements”, In Int Symp Computer Methods in Biomechanics and Biomedical Engineering (CMBBE), 2018.
[18-7] Burkhard M, Fürnstahl P, Farshad M. Three‑dimensionally printed vertebrae with different bone densities for surgical training. European Spine Journal, 2018. Accepted/in press.
[18-8] Roner S, Carrillo F, Vlachopoulos L, Schweizer A, Nagy L, Fürnstahl P. Improving accuracy of opening-wedge osteotomies of distal radius using a patient-specific ramp-guide technique. BMC musculoskeletal disorders, 2018. 19(1): 374.6.
[18-9] Vlachopoulos L, Carrillo F, Dünner C, Gerber C, Székely G, Fürnstahl P. A novel approach for the approximation of the humeral head retrotorsion based on three-dimensional registration of the bicipital groove. The Journal of Bone & Joint Surgery 2018. Accepted/in press.
[18-10] Vlachopoulos L, Lüthi M, Carrillo F, Gerber C, Székely G, Fürnstahl P. Restoration of the Patient-Specific Anatomy of the Proximal and Distal Humerus - Statistical Shape Modeling versus Contralateral Registration Method. The Journal of Bone & Joint Surgery 2018.